New Report Shows Bright Spots, Areas of Concern for Quality in Minnesota Public Health Insurance Programs
May 4, 2023
Disparities across payer types and within state insurance programs persist
Gaps in health care quality for people with coverage through Medical Assistance and MinnesotaCare compared to other types of health insurance persisted in 2021, according to a new report from MN Community Measurement (MNCM). The report was prepared for the Minnesota Department of Human Services and compares health care quality and health outcomes for people who received coverage through Minnesota Health Care Programs managed care organizations (MHCP MCO) to the same measures for people with private health insurance coverage or Medicare Advantage plans. The report includes 21 measures of health care quality for preventive care, chronic disease management, and mental health.
As health care disruptions due to the COVID-19 pandemic began to wane in 2021, many measures of health care quality started to rebound from the sharp declines that happened in 2020. As a result, several quality measures for MHCP MCO enrollees improved in 2021 — these included measures for colorectal cancer screening, controlling high blood pressure, optimal asthma control for adults, optimal diabetes care, and adolescent mental health screening. For these measures, performance gaps between MHCP MCOs and other payers have also narrowed or stayed the same over the past several years.
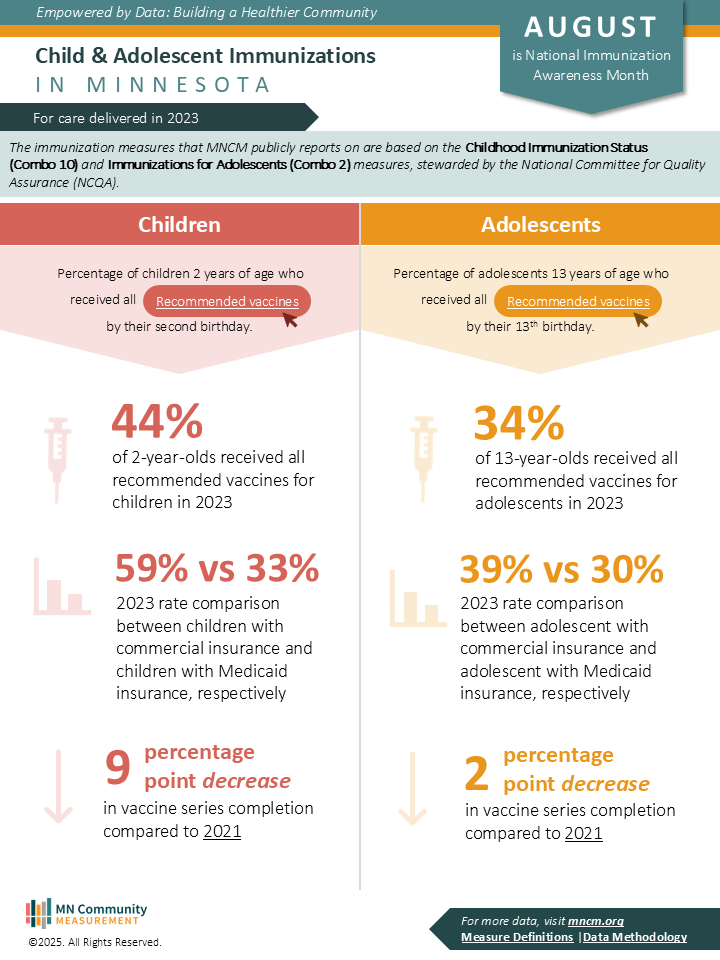
For breast cancer screening and childhood immunization, however, quality performance has been declining and gaps between MHCP MCO performance and other payer types have been widening over time. Just 54.4 percent of MHCP MCO enrollees were up to date on breast cancer screening in 2021, compared to 75.6 percent in the “other payers” comparison group. Among children who turned two years old in 2021, only 41.0 percent who had MHCP MCO coverage were up to date on recommended immunizations, compared to 67.6 percent with coverage through other payers.
The report also examines variation in quality within the MHCP MCO population, by race, ethnicity, language, and country of origin. Key findings related to variation within MHCP programs include significantly lower performance rates for Black and Indigenous/Native people, compared to other racial and ethnic groups. Of the 21 measures included in the report, rates were significantly lower for Black patients on 13 of the measures, and significantly lower for Indigenous/Native patients on 7 of the measures.
“Being able to measure and report on health care quality in this way really shines a light on where we are making progress and where additional strategies may be needed to improve outcomes for people who have health coverage through state programs,” said Julie Sonier, MNCM President and CEO. “While it’s encouraging to see progress in some areas, there is a long way to go to improve outcomes for people covered by these programs. For nearly all measures, tackling the gaps in outcomes will require innovative strategies and sustained focus to move the needle.”
Appendices to the report include quality results for patients enrolled in MHCP MCOs by medical group and clinic location , as well as details on the methodology for data collection and analysis.
About Minnesota Health Care Programs
Minnesota Health Care Programs include Medical Assistance, Minnesota’s Medicaid program, and MinnesotaCare. These public health care programs provide coverage to Minnesotans with low incomes who cannot afford private insurance. They currently collectively serve more than one million Minnesotans.
Posted in Press Release
Recent Posts