Uneven Progress, Mixed Results on Minnesota Health Disparities in 2022
October 26, 2023
New report provides data to support health equity improvement strategies
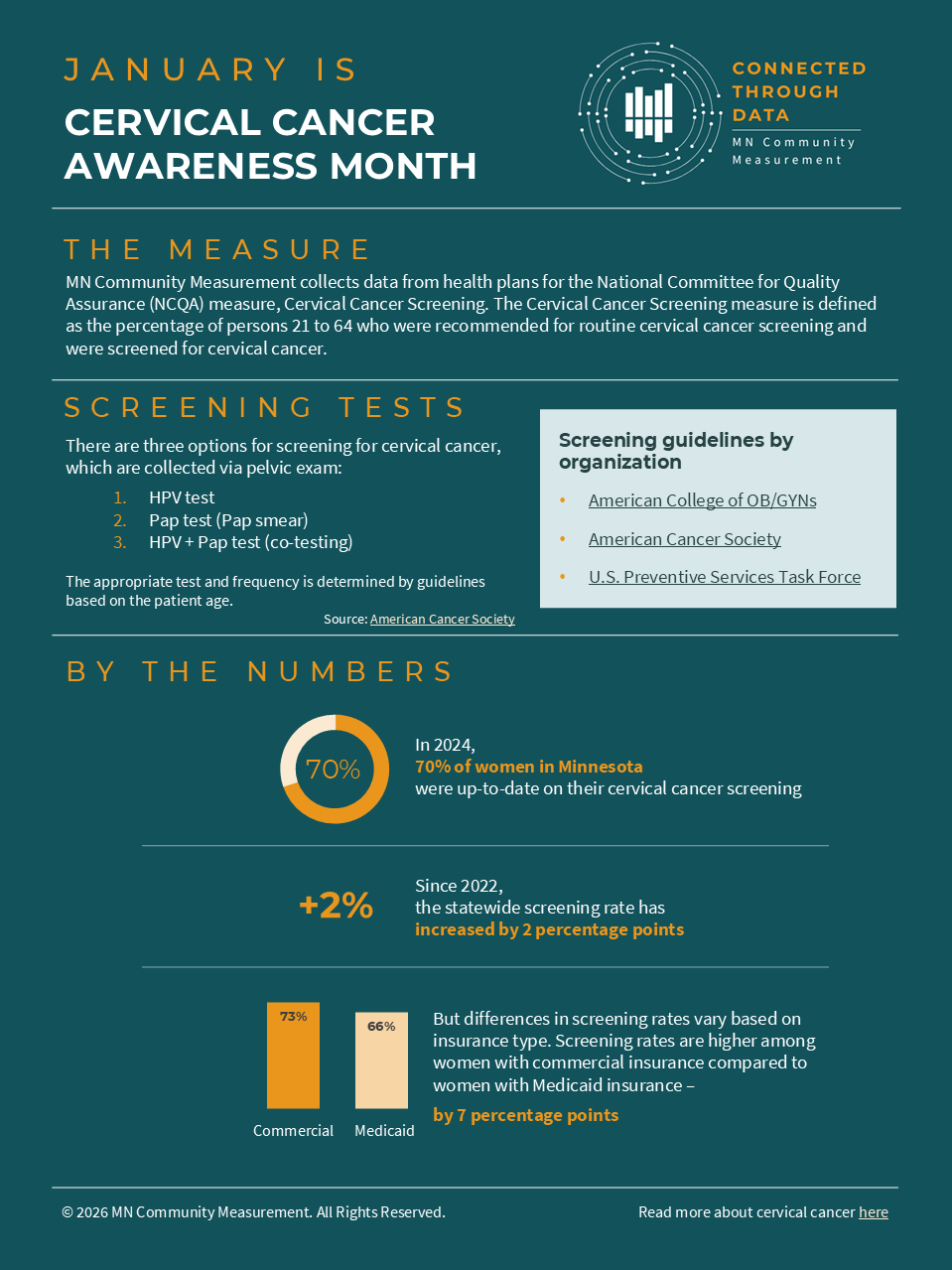
MN Community Measurement (MNCM), a nonprofit organization dedicated to collecting and reporting data on health care quality, cost, and equity to drive improvement in health care, has released its annual report on health care disparities by race, Hispanic ethnicity, language, and country of birth. The measures included in the report assess outcomes for diabetes, heart disease, asthma, and depression, along with preventive care screenings for cancer and adolescent mental health. Separate appendices to the report detail medical group level results by race/ethnicity, language, and country of origin.
Key Findings
The report documents continued wide disparities in health care quality and outcomes by race, ethnicity, language, and country of origin using data collected by MNCM in 2023 that reflects care provided in 2022. Key findings include the following:
- Groups that are most likely to have quality outcomes that are lower than the statewide average include people who are Black, Indigenous/Native, Hispanic/Latinx; people whose preferred language is Hmong, Somali, or Spanish; and people born in Laos, Mexico, or Somalia.
- In general, the measure with the largest disparities across subpopulations is colorectal cancer screening. This has important health and equity impacts, because colorectal cancer is the second leading cause of death from cancer in the U.S., and early detection and treatment is associated with higher survival and lower treatment cost.
- This year, MNCM’s data on disparities in colorectal cancer screening show that screening for nearly all the race, ethnicity, language, and country of origin groups fell compared to 2021. In part, this was due to incorporating a U.S. Preventive Services Task Force recommendation to begin screening at age 45 rather than 50.
- Even after adjusting for the impact of the new age range for screening, rates for many population subgroups fell in 2022. Two “bright spots” were improvements in rates for non-English speakers and people who identify as multi-racial.
- Except for colorectal cancer screening, 2022 rates for most subpopulations were significantly higher or not statistically different than 2021 rates. Notable exceptions were declining rates for optimal vascular care and optimal asthma control for children among people who are White, Not Hispanic/Latinx, English speakers, or U.S.-born.
- 2022 results for most health care quality measures remained statistically below pre-pandemic (2019) baselines for most population subgroups. One notable exception was the measure for adolescent mental health and/or depression screening, where 11 of 12 subpopulations had a rate that was higher than their 2019 rate.
- There is wide variation in health care quality measure results across medical groups and across subpopulations. Some medical groups achieved above average outcomes across patient subpopulations, while others had substantial variation in outcomes.
Implications of this Report
“In many ways, this report provides a roadmap for organizations like health plans, health care providers, employers, community groups, and others to show how they can focus their efforts to improve health equity,” said Julie Sonier, President and CEO of MNCM. For example, contractual incentives can be an effective tool for reducing disparities within medical groups. Investing in structural capacity to analyze and address disparities, including partnerships with community-based organizations, has the potential to address barriers to optimal outcomes and to reduce disparities. For measures like colorectal cancer screening, targeted education and outreach campaigns by community groups and employers about the importance of screening are also promising strategies to reduce disparities.
“As an organization that brings together data from across the state to drive improvement in health care, MNCM is proud of the role that we play in shining a spotlight on disparities and helping to drive improvement,” said Sonier. “The data that we produce calls attention to this important issue and helps to drive investment on many fronts to make progress toward health equity.”
Importance of Measurement
Measuring and reporting on health care quality and disparities in outcomes helps consumers understand how care varies across providers, allows providers to identify improvement opportunities and how their measures compare to others, and helps health plans and other purchasers better understand and improve value for money that is spent on health care.
“Minnesota is unique in the capabilities that we’ve built to measure and report on health care outcomes,” said Sonier. “Having a common set of priorities and a common trusted source of data have been huge assets to Minnesota in focusing efforts to drive improvement.”
Posted in Press Release
Recent Posts