Empowered by Data: A Collaborative Approach to Addressing Gaps in Diabetes Care

MN Community Measurement
November is American Diabetes Month. In the United States, diabetes affects more than 11% of the population, or about 38 million people.1 In Minnesota, approximately 10.5% of residents, or about 470,000 have diabetes (type 1 or 2)2. Beyond the condition itself, people with diabetes have a higher risk of additional health conditions, including kidney disease and heart disease.2
Diabetes also disproportionately impacts certain communities, with higher prevalence in Indigenous/Native and Black adults, as well as those with lower incomes. 1,2 A collaborative effort across community partners, including local and state public health, health systems, health plans, community pharmacists, and community organizations, are essential to addressing the gaps in care and improving care for all Americans with diabetes.
The Optimal Diabetes Care Measure
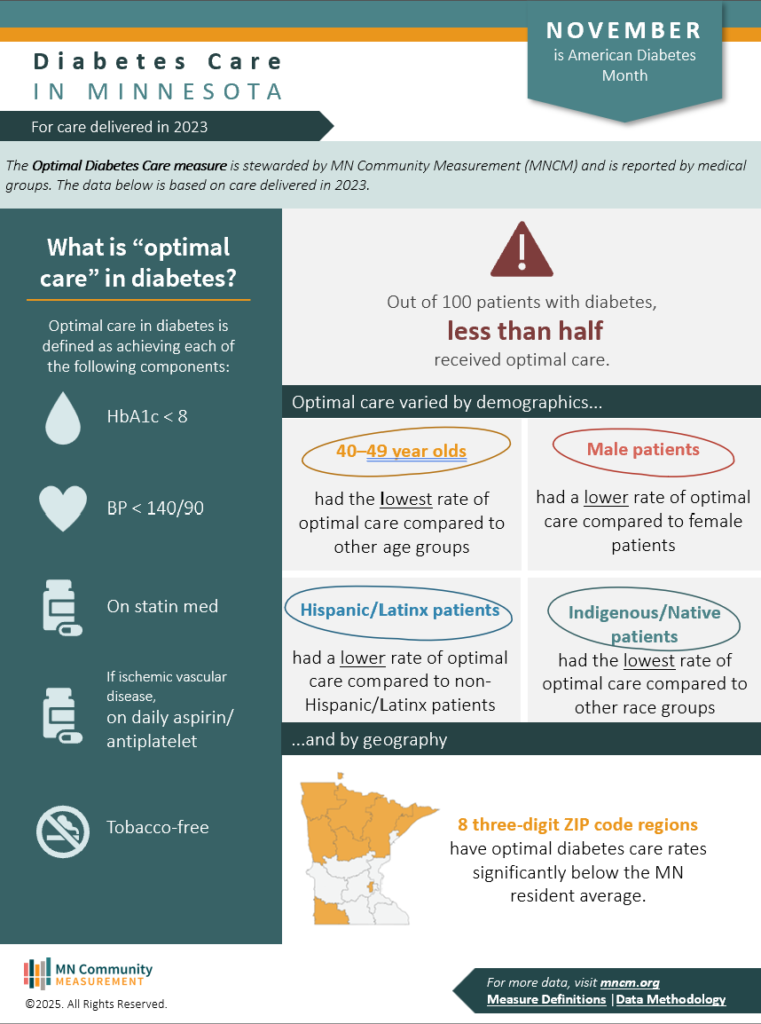
The Optimal Diabetes Care measure, stewarded by MN Community Measurement (MNCM), is a composite measure that assesses the percentage of adults 18-75 years of age who had a diabetes diagnosis (type 1 or 2) and whose diabetes was optimally managed as defined by achieving all of the following components:
- HbA1c less than 8
- BP less than 140/90
- On a statin medication (unless contraindicated)
- On a daily aspirin (if there is a co-morbidity of ischemic vascular disease)
- Tobacco-free
What the Data Shows
The data for this measure are aggregated and reported to MNCM by medical groups. Analyses of this measure showed:
- In 2023, 46.3% of patients with diabetes met all five of the components described above.
- 40–49-year-olds with diabetes had the lowest rate of optimal care compared to other age groups.
- Male patients with diabetes had lower rates of optimal care compared to female patients.
- Hispanic/Latinx patients with diabetes had lower rates of optimal care compared to non-Hispanic/Latinx patients.
- Indigenous/Native patients had the lowest rate of optimal care compared to other race groups.
Improving Diabetes Care Through Collaboration
MNCM held a virtual panel on Wednesday, September 24th, where diabetes experts explored the essential role of partnerships for improving diabetes care. Panelists included Gregg Simonson, PhD (HealthPartners International Diabetes Center), Anders Carlson, MD (HealthPartners International Diabetes Center), Bridget Ideker, RD, LD, CHWC (Minnesota Department of Health), and Sara Maki, PharmD, BCACP (Mass General Hospital).
Below is a summary of the panel discussion –
Barriers to care
- Understanding social determinants of health: There are persistent disparities seen at all levels of the diabetes care continuum. As Bridget Ideker noted, “80% of your health happens outside of the clinical wall”, emphasizing the importance of understanding social determinants of health and the role they play in patient outcomes.
- Accessing primary care: Accessing primary care can be a challenge for patients, particularly those living in rural areas. Engaging the whole health care team can help bridge the gap and promote patient accountability. Many patients want to be engaged with their care, but scheduling appointments can be difficult.
- Medication & technology costs: Innovations such as GLPs and continuous glucose monitoring (CGM) systems have drastically improved diabetes care. However, their high cost can lead providers to unintentionally “gatekeep” information on these options for their patients. Instead, providers should offer information on these tools, support patients to make informed choices, and help connect them to clinic and community resources, such as dietitians, diabetes educators, and pharmacists, to help navigate access and affordability.
Successful Partnership Examples
The panelists shared examples of successful partnerships that have strengthened diabetes care, including:
- Improving access to insulin through Minnesota’s Insulin Safety Net Program
- Partnering with community organizations to provide cooking classes using healthy, locally available food in the Boston area (Healthy Chelsea coalition)
- Hosting community conversations to better understand community-specific needs, including:
Using Partnerships to Address Disparities
The panelists also discussed how to use partnerships to address disparities in diabetes care:
- Incorporating social risk factor screenings in a clinic visit to connect patients to community resources.
- Using telehealth and remote monitoring through CGMs to help navigate transportation, work, and childcare barriers that may prevent patients from showing up at their appointments.
- Engaging community health workers, who serve as trusted patient connectors between primary care and community organizations for patients.
Why This Matters
Persistent disparities in diabetes care highlight the critical need for strong partnerships between clinicians and the community. Meeting patients where they are and connecting them with relevant community resources empowers them to make informed decisions and take an active role in managing their health. These partnerships also support clinicians by ensuring they are not working in isolation—creating a shared, collaborative effort to improve diabetes outcomes.
Sources
- American Diabetes Association. Statistics About Diabetes. Retrieved from https://diabetes.org/about-diabetes/statistics/about-diabetes
- Minnesota Department of Health (2025). Diabetes in Minnesota. Retrieved from https://www.health.state.mn.us/diseases/diabetes/data/diabetesfacts.html
