Empowered by Data: Spotlight on Screening for Sexual Health

September is Sexual Health Awareness Month. As we close out September, we’re highlighting two of the measures we report on – Cervical Cancer Screening and Chlamydia Screening in Women.
Cervical cancer, once one of the most common cancers affecting women in the United States, has significantly decreased since the 1970s. The reason for the decline can mainly be attributed to routine cervical cancer screenings, which can be done through routine Pap smears and HPV tests.1,2 In recent years, there has also been a notable decrease in cervical cancer rates among women between the ages of 20 and 24, and is likely a result of the introduction of the HPV vaccine series.1 While the human papillomavirus (HPV) is not the only cause of cervical cancer, it is considered the most important risk factor and accounts for nine of out ten cervical cancer cases.3,4 HPV is a very common virus, spread through skin-to-skin contact, including sexual activity, and affects approximately 13 million people each year.3,5 Fortunately, the HPV vaccine has been found to prevent more than 90% of cancers caused by HPV, including cervical cancer.4,5
Chlamydia, a common and treatable bacterial infection, is also spread through sexual contact with an infected partner.6 Individuals can be infected with chlamydia without showing symptoms, making it difficult to diagnose on symptoms alone.7 Additionally, repeat infections are also possible.7 If left untreated, chlamydia can cause pelvic inflammatory disease in women, which can lead to complications such as ectopic pregnancy, infertility, and chronic pelvic/abdominal pain.7 The most effective way to diagnose chlamydia and prevent long-term complications is through recommended urine tests or vaginal swabs.7 Fortunately, cases have declined 8% across the United States since 2023.8
Measure Definitions
Both measures are stewarded by the National Committee for Quality Assurance (NCQA). Below are the measure definitions:
- Cervical Cancer Screening: Assesses women who were screened for cervical cancer using any of the following criteria:
- Women 21-64 years of age who had cervical cytology performed within the last 3 years.
- Women 30-64 years of age who had cervical high-risk human papillomavirus (hrHPV) testing performed within the last 5 years.
- Women 30-64 years of age who had cervical cytology/high-risk human papillomavirus (hrHPV) cotesting within the last 5 years.
- Chlamydia Screening in Women: Percentage of persons 16-24 years of age who were recommended for routine chlamydia screening, were identified as sexually active, and had at least one test for chlamydia during the measurement period.
What the data shows
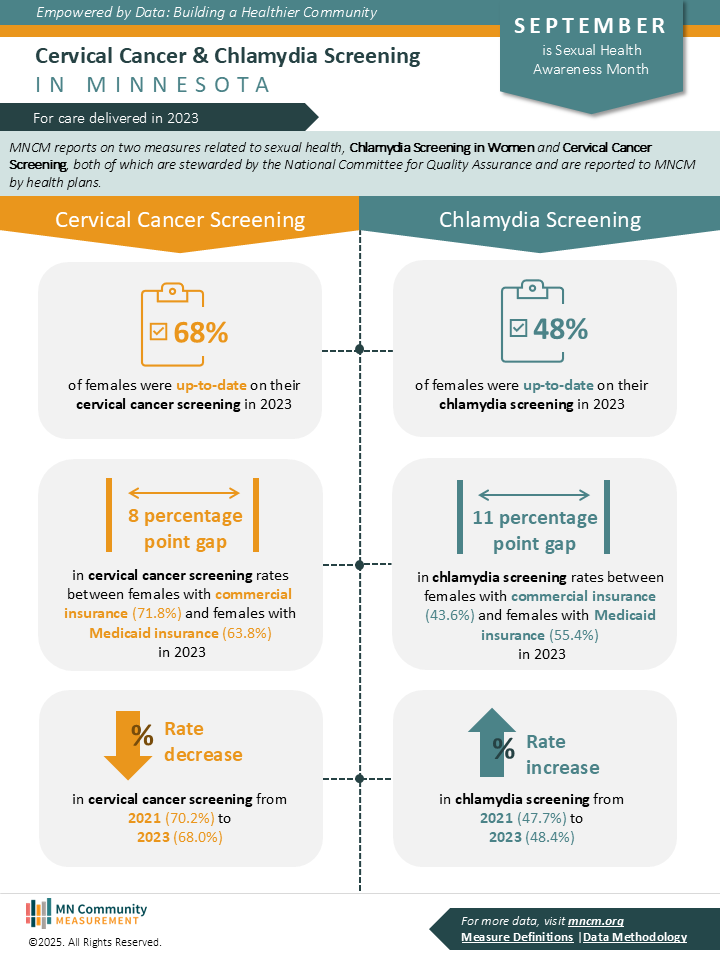
The data for these measures are aggregated and reported to MNCM by health plans. Analyses of these measures show:
Cervical Cancer Screening
- The number of women with an up-to-date cervical cancer screening has decreased slightly in 2023 compared to 2021: 68.0% and 70.2%, respectively.
- Women with commercial insurance coverage had a higher rate of screening compared to women with Medicaid coverage: 71.8% and 63.8%, respectively.
Chlamydia Screening
- The number of women who received a recommended chlamydia screening has increased slightly in 2023 compared to 2021: 48.4% and 47.7%, respectively.
- Women with Medicaid coverage had a higher rate of screening compared to women with commercial insurance coverage: 55.4% and 43.6%, respectively.
Why This Matters
Despite the advances in cervical cancer prevention and chlamydia screening, there is still work to be done. In the case of cervical cancer screening, approximately 32% of women between the ages of 21 and 64 were missing an updated cervical cancer screening in 2023. And, even more desperate, approximately 52% of sexually active women between the ages of 16 and 24 received a recommended chlamydia screening in 2023.
But this work does not lie solely on the shoulders of providers and health systems. Rather, a collaborative effort is needed not only to raise awareness on the importance of screening, but to also provide education on preventive efforts such as vaccination and safe sex practices. Empowering patients with data, fostering open and non-judgmental conversation, and providing community resources such as where to receive low-cost vaccines or free, confidential STI testing can be incredibly valuable. Evidence-based knowledge is power.
And it is important to note that while the measures discussed here are specific to female patients, sexual health is applicable to everyone – all sexes, gender identities, sexual orientations, and demographic groups.
Rethinking the Chlamydia Screening in Women Measure
MNCM’s Measurement and Reporting Committee (MARC) reviewed the Chlamydia Screening in Women measure in March 2025. Members expressed concerns with the how the measure identifies sexually active patients (i.e., through use of oral contraception as a proxy), and the exclusion of male patients. Ultimately, the committee recommended that a public comment be submitted to NCQA with the recommended changes, which will be drafted in the next few months. If your organization has any specific comments related to the measure, please email publiccomment@mncm.org.
Resources for Cervical Cancer
General Information
- American Cancer Society (ACS)
- Centers for Disease Control & Prevention (CDC)
- Minnesota Department of Health (MDH)
- Planned Parenthood
HPV Vaccination Resources
Find vaccination resources near year.
Resources for Chlamydia
General Information
- Centers for Disease Control & Prevention (CDC)
- Minnesota Department of Health (MDH)
- Planned Parenthood
Get Tested
Find testing resources near you.
Sources
- American Cancer Society (2025). Risk Factors for Cervical Cancer. Cervical Cancer. Retrieved from https://www.cancer.org/cancer/types/cervical-cancer/causes-risks-prevention/risk-factors.html
- American Cancer Society (2025). Cervical Cancer Early Detection, Diagnosis, and Staging. Cervical Cancer. Retrieved from https://www.cancer.org/cancer/types/cervical-cancer/detection-diagnosis-staging.html
- American Cancer Society (2025). Key Statistics for Cervical Cancer. About Cervical Cancer. Retrieved from https://www.cancer.org/cancer/types/cervical-cancer/about/key-statistics.html
- Centers for Disease Control & Prevention (2025). Cancers Caused by HPV. Human Papillomavirus (HPV). Retrieved from https://www.cdc.gov/hpv/about/cancers-caused-by-hpv.html
- Centers for Disease Control & Prevention (2024). HPV Vaccination. Human Papillomavirus (HPV). Retrieved from https://www.cdc.gov/hpv/vaccines/
- Planned Parenthood. Chlamydia. Retrieved from: https://www.plannedparenthood.org/learn/stds-hiv-safer-sex/chlamydia
- Centers for Disease Control & Prevention (2025). About Chlamydia. Sexually Transmitted Infections. Retrieved from https://www.cdc.gov/chlamydia/about/
- Centers for Disease Control & Prevention (2025). Sexually Transmitted Infections Surveillance, 2024 (Provisional). Sexually Transmitted Infections. Retrieved from https://www.cdc.gov/sti-statistics/annual/index.html#cdc_research_or_data_summary_findings-highlights