Empowered by Data: Uncovering Screening Disparities and Reducing Breast Cancer Risk

American Cancer Society

MN Community Measurement
This October marks the 40th anniversary of Breast Cancer Awareness Month. According to the American Cancer Society, about 1 in 8 women will be diagnosed with invasive breast cancer in their lifetime. Fortunately, however, early detection through screening and advances in treatment have decreased mortality by 44% since 1989. Screening can catch cancer early, when it is easier to treat. When caught early, the five-year survival rate is approximately 99% compared to 32% when caught in the later stages.1 Despite these findings, significant racial disparities exist in both breast cancer screening and mortality. In Minnesota, although the incidence of breast cancer is higher in white women, breast cancer mortality is highest among American Indian and African American women.2
Measure Definitions
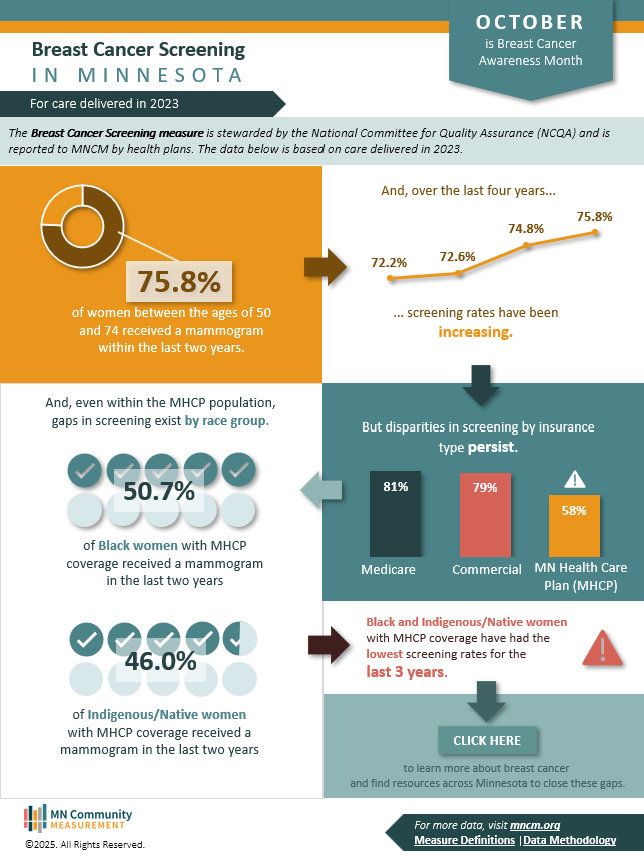
The Breast Cancer Screening measure that is the focus of October’s infographic is stewarded by the National Committee for Quality Assurance (NCQA). The data are aggregated and reported to MN Community Measurement (MNCM) by health plans across the state.
For the 2023 measurement year, the measure is defined as the percentage of women between the ages of 50 and 74 who received a mammogram in the past two years.3
What the Data Shows
MNCM’s data show that 75.8% of Minnesota women between the ages of 50 and 74 received a mammogram within the last two years in 2023. However, screening is not equal across the population. Approximately 58% of women with MHCP insurance received a mammogram in 2023, compared to 80% of women with either commercial or Medicare coverage. Persistent disparities exist even within the MHCP population, where, over the last three years, Black and Indigenous/Native women have significantly lower rates of screening compared to the MHCP average.
Social Determinants of Health & Breast Cancer
Social determinants of health such as access to transportation, health insurance coverage, and the cost of health care can create significant barriers to both breast cancer screening and treatment for certain populations. Addressing these social determinants of health is essential for developing breast cancer screening programs, interventions, and policies that target populations most in need of improved outcomes. This interactive dashboard from MDH illustrates how selected social determinants of health impact both breast cancer burden (incidence and mortality) and screening rates in Minnesota. This tool is designed to support program planning, decision making, and resource allocation. The resource section at the end of this page includes links to additional data sources, as well as background information on social determinants of health.
Understanding Risk Factors
Some risk factors for breast cancer are things you cannot change, such as getting older or inheriting certain gene changes. These make your risk of breast cancer higher. But certain breast cancer risk factors can be modifiable and are related to personal behaviors, and include:
- Physical activity: Evidence is growing that regular physical activity reduces breast cancer risk, especially in women past menopause. The main question is how much activity is needed. Some studies have found that even as little as a couple of hours a week might be helpful, although more seems to be better. Exactly how physical activity might reduce breast cancer risk isn’t clear, but it may be due to its effects on body weight, inflammation, and hormone levels.
- Alcohol consumption: Drinking alcohol is another modifiable risk factor that is clearly linked to an increased risk of breast cancer.4 The risk increases with the amount of alcohol consumed. Women who have 1 alcoholic drink a day have a small (about 7% to 10%) increase in risk compared with those who don’t drink, while women who have 2 to 3 drinks a day have about a 20% higher risk.
Other lifestyle-related risk factors include decisions about having children and taking medicines that contain hormones. You can learn more about risk factors by visiting the American Cancer Society website.
Why This Matters
While significant progress has been made in both the screening and treatment of breast cancer in the last decade, there is still more work to do. A collaborative and culturally tailored effort from health care providers, payers, community organizers, and local public health is essential to address the disparities and barriers that persist in breast cancer screening.
Resources
- ACS CancerRisk360 Assessment: Assessment tool from the American Cancer Society to learn more about what you can change to improve your health and lower your cancer risk.
- African American Breast Cancer Alliance: Nonprofit organization dedicated to providing culturally tailored education, resources, advocacy, and support for Black individuals and families affected by breast cancer.
- American Indian Cancer Foundation: National, Native-governed nonprofit dedicated to eliminating cancer disparities among Indigenous people by improving access to prevention, early detection, treatment, and survivor support.
- Breast Cancer Education Association: Volunteer-run Minnesota nonprofit that provides information, support, and resources for those affected by breast cancer.
- Breast Cancer GAPS Project: Nonprofit organization dedicated to reducing breast cancer disparities among Black women by partnering with communities and providers to ensure equitable care.
- MDH Sage Program: Information on access to breast cancer screening for low-income or uninsured Minnesotans.
- National Breast Cancer Roundtable: National coalition of member organizations established by the American Cancer Society dedicated to ensuring that everyone understands breast cancer risk and screening and has access to timely, high-quality, and compassionate care.
Sources
- American Cancer Society (2018). Breast Cancer Statistics. Retrieved from https://cancerstatisticscenter.cancer.org/types/breast
- Minnesota Department of Health (2020). Breast cancer disparities in Minnesota women. Retrieved from https://www.health.state.mn.us/data/mcrs/docs/breastfs.pdf
- National Committee for Quality Assurance. Breast Cancer Screening (BCS). Retrieved from https://www.ncqa.org/report-cards/health-plans/state-of-health-care-quality-report/breast-cancer-screening-bcs/
- American Cancer Society (2025). Alcohol Use and Cancer. Retrieved from https://www.cancer.org/cancer/risk-prevention/diet-physical-activity/alcohol-use-and-cancer.html