Collaborate. Empower.
Improve.
Better health care starts with better health information. At MNCM, we bring providers, payers, and community partners together to improve quality, equity, and affordability in Minnesota —
so everyone benefits.
About Us
Our Vision
At MN Community Measurement, we believe data is powerful and we’re using it to lead the improvement of health care in our region. We work with doctors, hospitals, clinics, insurance companies, purchasers, and state agencies to design measures. We then collect, analyze, and share actionable data on health care quality and cost.
Our Services
MNCM serves the health care community by:
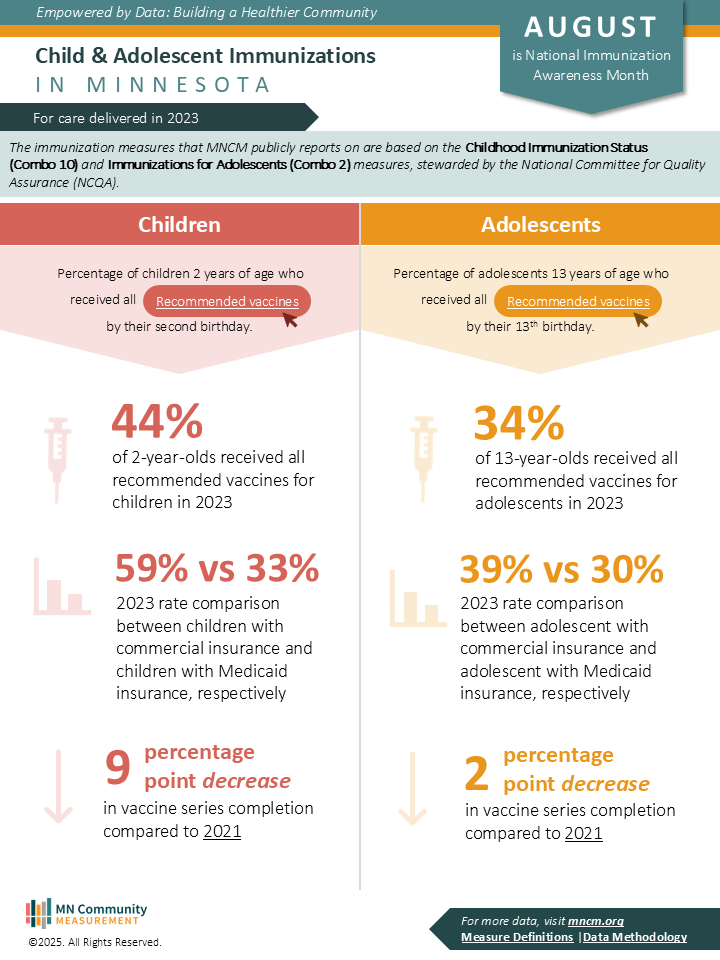
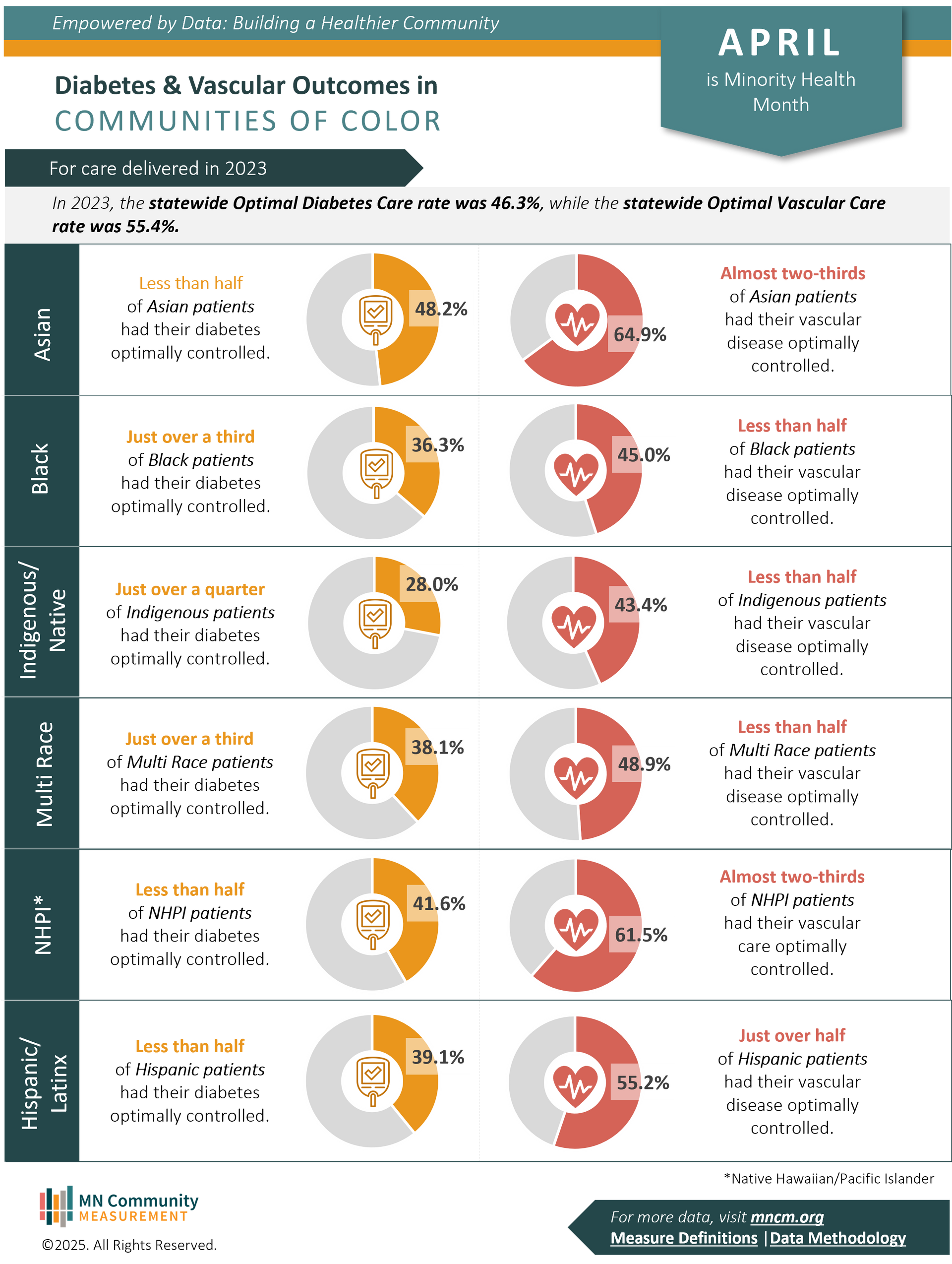
- Delivering trusted data on health care quality and cost
- Collaborating on measures with providers and payers.
- Publishing reports that reveal trends and opportunities.
- Empowering patients with MNHealthScores comparisons.
- Engaging members to advance affordable, equitable care.
Our Data
MNCM offers a variety of publicly available data analysis tools to support the community in its efforts to improve health care in Minnesota. Click on the links below to learn more:
What's New
Blog Posts