Analyzing Trends in Colorectal Cancer Screening Rates: Insights and Impacts
November 11, 2024
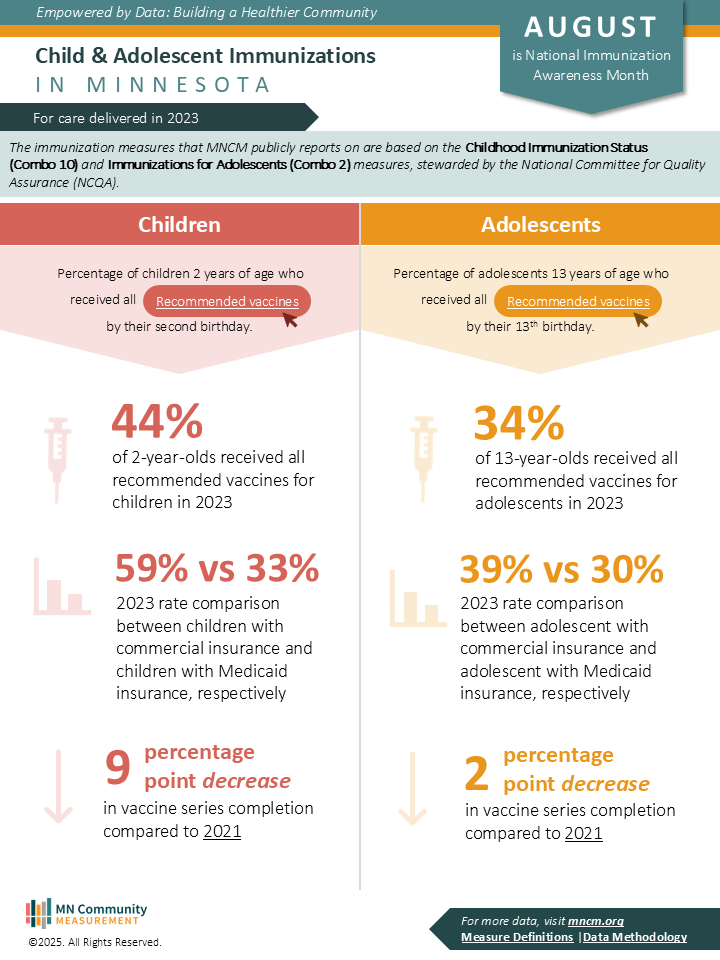
2022 measurement year
Colorectal cancer screening is a crucial preventive measure, especially given that early detection significantly increases treatment success. One of the clinical quality measures MN Community Measurement reports on is based on NCQA’s HEDIS measure for colorectal cancer screening. In this post, we’ll dive into the 2022 data on screening rates, the impacts of changing eligibility guidelines, and disparities across demographics.
On November 12 , the Minnesota Department of Health , the Minnesota Cancer Alliance , and the American Cancer Society will co-host a meeting to bring together health care payors, providers, and patient advocates. This event will focus on ways to increase cancer screening through coordinated strategies, including presentations and collaborative small-group discussions.
One highlight will be a presentation by MNCM’s Jess Donovan on colorectal cancer screening insights from the 2022 annual reports. Jess joined MNCM in 2017 and brings a unique blend of clinical and public health expertise to her role. Starting as a Project Coordinator focused on clinical data validation and analysis, Jess transitioned to the role of Clinical Measurement Analyst in 2018, where she now specializes in data analysis of clinical quality measures and data visualizations. Jess holds a master’s in public health with a focus in epidemiology from the University of Minnesota and is a Registered Nurse.
Understanding the Colorectal Cancer Screening Measure
The colorectal cancer screening measure targets adults aged 45 to 75 who are up-to-date with recommended screenings. Acceptable tests include colonoscopy, sigmoidoscopy, CT colonography, and stool blood tests. By analyzing patient-level data submitted to us by medical groups, we can assess screening rates across age, race, language, geographic location, and insurance type, providing valuable insights for tailoring public health efforts.
How Have Screening Rates Changed Over Time?
Since 2019, we’ve observed shifts in statewide screening rates. Expectedly, the pandemic caused a significant drop in screenings during 2020, with rates recovering slightly in 2021. However, in 2022, screening rates fell again to 67.8%. This decrease aligned with NCQA’s adjustment of the eligibility age from 50–75 to 45–75, which likely contributed to the decline, especially as the younger age group (45-49) had not yet been regularly screened.
We recalculated the 2022 rate using only the 50–75 age group and found that rates were closer to pre-2022 levels but still below the 2021 mark. This suggests that while the age expansion affected the decline, other factors may have also played a role—such as the challenges of scheduling colonoscopies as people returned to in-office work.
Figure 1: Three-Digit ZIP Code Analysis
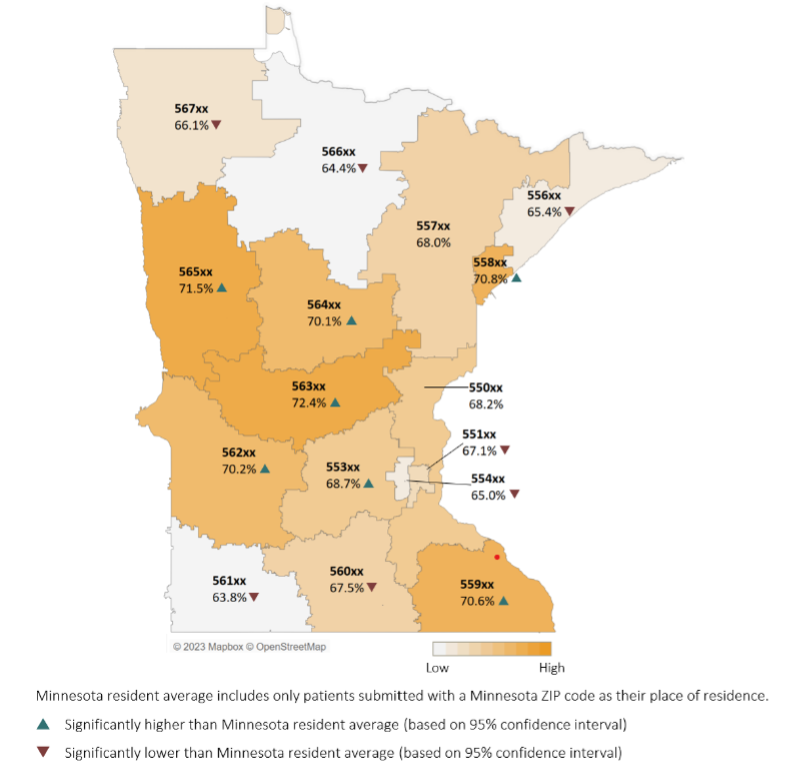
Minnesota Health Care Quality Report – Part 1: Clinical Quality Measures Reported by Medical Groups (results for care delivered in 2022)
Exploring Geographic and Demographic Variations
Our geographic analysis (Figure 1) highlights significant variations in screening rates across Minnesota’s ZIP codes. We used a Minnesota-resident average (68.0%), rather than a statewide average (67.8%), for a more localized comparison. In general, areas with darker color-coding on our maps indicate higher screening rates, while lighter areas show lower participation. Three-digit ZIP code regions with higher than average rates of screening include: 553, 558, 559, 562, 563, 564, and 565.
Looking at demographic breakdowns (Figure 2), our health disparities reports reveal important trends:
- Race and Ethnicity : In 2022, screening rates were consistently lower across race groups, except for the white population. For Hispanic/Latinx populations, screening rates also fell below the statewide average. We also analyzed screening rate trends across racial groups and found that, except for the multi-race group, whose rates remained stable, all groups had significantly lower screening rates in 2022 compared to both 2021 and 2019.
- Language : In 2022, English-speaking patients had significantly higher screening rates compared to the statewide average, while patients who spoke Hmong, Somali, or Spanish has significantly lower rates. When we analyzed trends by splitting the population into English-speaking and non-English-speaking groups, both showed substantial declines in 2022 compared to pre-pandemic levels (2019).
- Country of Origin : We also examined patients by country of origin, finding that U.S.-born patients had higher screening rates, while those from Laos, Mexico, and Somalia had lower rates than the statewide average.
Figure 2: Trend by RELC Subpopulations
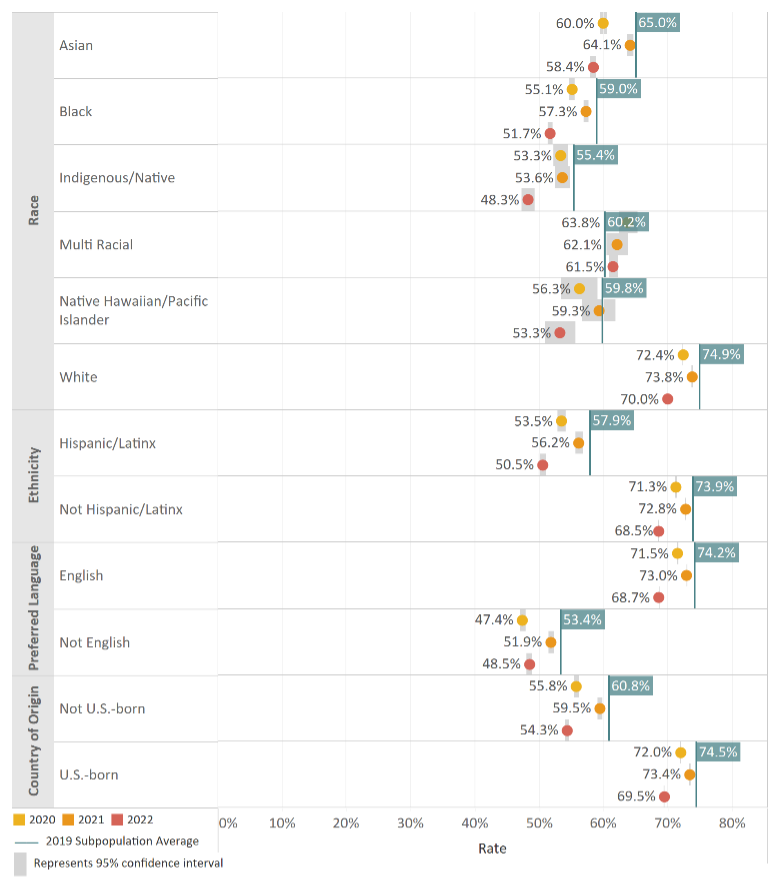
Minnesota Health Care Disparities by Race, Ethnicity, Preferred Language, and Country of Origin (Results for care delivered in 2022)
The Influence of Insurance Type
Another crucial factor in screening rates is insurance type . Our data on Minnesota Health Care Program (MHCP) patients show a consistent gap in screening rates between those with MHCP and those with commercial or Medicare insurance. Although both groups experienced declines in 2022, the gap remained. Within the MHCP population, age breakdowns revealed a low screening rate for the newly eligible 45–49 age group, consistent with the findings at the statewide level.
Health Disparities Within the MHCP Population
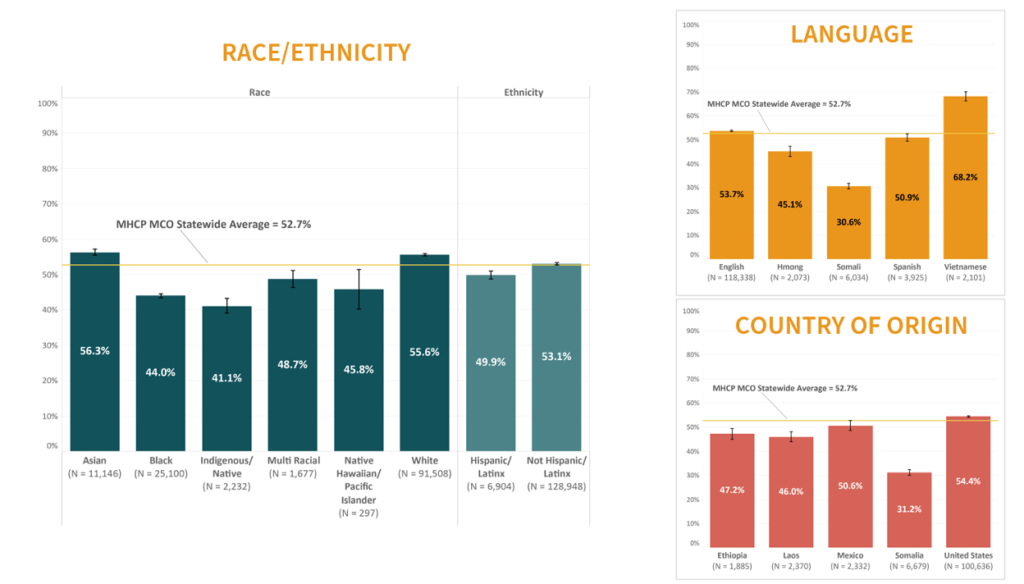
Our 2022 analysis for MHCP populations showed disparities across race, ethnicity, language, and country of origin (Figure 3):
- Race and Ethnicity : In comparison to the statewide MHCP screening rate, rates were higher among Asian and White MHCP patients, while lower rates were observed for Black, Indigenous, Multi-race, Native Hawaiian, and Hispanic/Latinx groups.
- Language and Country of Origin : Among MHCP patients, those speaking Vietnamese or English had higher screening rates, while Hmong and Somali speakers had significantly lower rates in comparison to the statewide MHCP rate. Similarly, patients born in the U.S. had higher rates, while those from Ethiopia, Laos, and Somalia had lower rates.
Figure 3: Colorectal Cancer Screening Rates among MHCP Patients by RELC
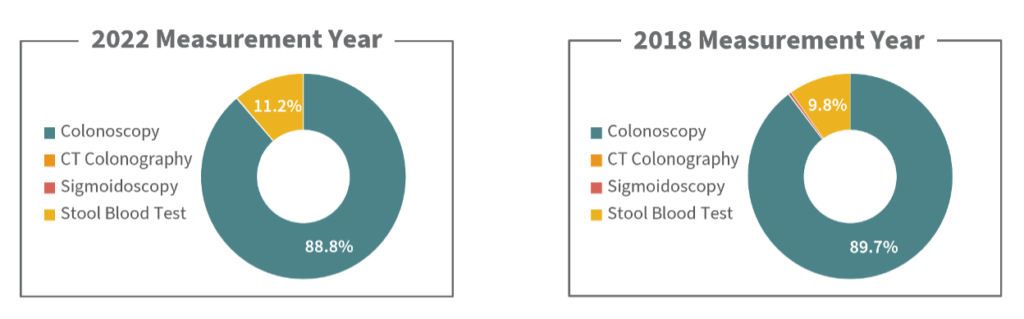
Screening Methods: Trends in Test Choice (Figure 4) In 2018, we analyzed screening types, revealing that colonoscopy was the most popular option among patients up-to-date on screenings. For the 2022 data, colonoscopy remains the most common method, though stool blood tests saw a slight increase, from about 10% to just over 11%. Increased awareness of this less-invasive option and possible logistical challenges of colonoscopy may explain the shift.
Figure 4: Screening Test Usage
Moving Forward: Addressing Disparities and Encouraging Screening
As we continue to assess colorectal cancer screening data, identifying the root causes of disparities and screening rate drops remains a priority. Our ongoing efforts aim to provide actionable insights, particularly as both patients and providers adapt to recent guideline changes. By targeting outreach and resources to underserved populations, we can help close these gaps, ultimately increasing preventive care for all.
Posted in Blog
Recent Posts